This article appeared in “Standing Tall for Justice,” an issue that received a 2023 Gold Award for Excellence from the Group on Institutional Advancement (GIA) of the Association of American Medical Colleges (AAMC). It also received a 2023 AAMC GIA Robert G. Fenley Writing Award.]
What You Will Learn:
- Race-based algorithms in clinical care have caused health disparities for people of color.
- Mass General Brigham leaders are rooting out biased race adjustments and other racial inequities in healthcare.
- Key to this effort is thinking about health equity as a quality and safety issue.
Prologue
In July 2012, Audrey* logged into her patient portal following her annual physical, as she had done for years.
A middle-aged white woman in good health, Audrey was pleased by the array of test results confirming her well-being. But then, in small print under one result, she noticed something strange related to an eGFR test: “If patient is black, multiply by 1.21.”
Audrey wondered, “What is eGFR? Why would it be different only for Black people? Who decides who’s Black?”
*Patient’s name has been changed to protect privacy.
Separate and unequal kidney medicine
“Every system is perfectly designed to get the results it gets.”
– Paul Batalden, MD, senior fellow, Institute for Healthcare Improvement
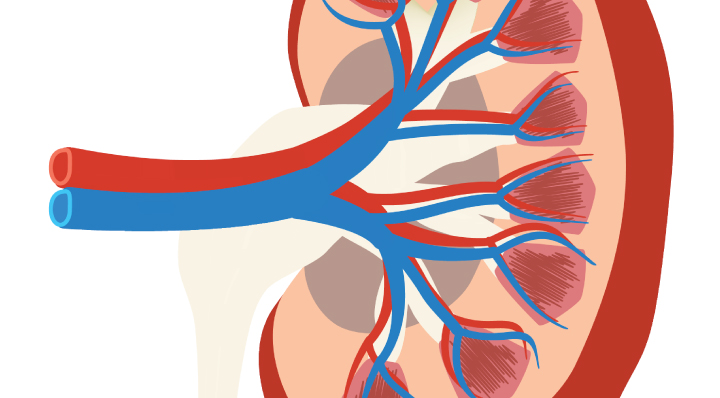
The eGFR is a blood test result estimating the glomerular filtration rate (GFR), which shows how well kidneys are filtering our blood. Because kidney function is difficult to evaluate with precision, accuracy, and speed, eGFR is a fast, inexpensive way for doctors to assess the health of these vital organs and determine if additional testing is needed.
The first method for estimating GFR through a blood test was developed in the 1970s but created from a study of 249 white men. In 1999, a new method for estimating GFR was introduced from a study of 1,628 participants, 12% of whom were Black. This method included a race adjustment, partly justified by a theory that Black people have more muscle mass than white people. This new approach to estimating GFR became a widely used standard of care in the U.S., even though it increased Black people’s GFR values by 21% (higher values indicate better kidney function).
“It’s interesting because these two studies introducing race adjustments in estimates of kidney function [the first in 1999 and a revision in 2009] were considered landmark, gold-standard studies at the time,” says Mallika Mendu, MD, MBA, nephrologist and executive medical director of clinical operations at Brigham and Women’s Hospital. “Both attempted to be inclusive of patients from different racial backgrounds, which was a huge improvement over prior studies that had been more homogeneous.”
Mendu adds, “I was taught the race adjustment in medical school in 2004, and then as a resident, and then as a fellow. And, to be frank, I didn’t question it.”
But Mendu’s perspective changed when she began practicing.
“I thought I needed to be transparent with my patients about the race adjustment,” she says. “And when I met with my patients and said it out loud, I found it confusing and hard to explain. So I stopped using it for my patients.”

Questions can change patient care
“If you are free, you need to free somebody else. If you have some power, then your job is to empower somebody else.”
– Toni Morrison, author
A decade after Mendu began medical school, racial justice and health equity movements began to take hold in academic medical centers across the U.S.
In 2016, Cameron Nutt, MD, was in his first year at Harvard Medical School (HMS) when he learned about the race adjustment for eGFR from his professor, Melanie Hoenig, MD, a nephrologist at Beth Israel Deaconess Medical Center (BI). Nutt and other students in the HMS Racial Justice Coalition asked Hoenig why the formula inflates Black people’s kidney function when they are at the greatest risk for kidney disease of any racial group.
“Even though racialized eGFR reporting was standard practice in nephrology, Dr. Hoenig never got defensive with students asking questions,” says Nutt. “She listened thoughtfully to our concerns. Then she set up meetings for us with other nephrologists at the BI and with pathologists who ran their lab. And after a long process and many conversations led by Dr. Hoenig, the BI changed their policy in March 2017 to stop reporting inflated eGFR values for Black patients.”
When Nutt joined the Brigham as an internal medicine resident in 2019, he wanted to learn more about the possible contribution of racialized eGFR reporting to racial disparities in the treatment of chronic kidney disease (CKD). Nutt joined a research team led by Mendu and her colleague, Salman Ahmed, MD, MPH, to analyze the records of more than 56,000 patients with CKD across Partners HealthCare (now Mass General Brigham).
When the researchers removed the race adjustment and reclassified the severity of CKD for the 2,225 who self-identified as Black or African American, 743 people (33%) met the criteria for a more severe stage of CKD. Of those, 64 met the criteria to be referred for kidney transplant—but because their scores had been adjusted for race, none of them had been waitlisted, evaluated, or even referred for a kidney transplant.
“Our research countered current practice by putting the facts out there, and this was only for our system,” says Mendu. “Across the country, Black patients are three times more likely to progress from chronic kidney disease to kidney failure. And they are less likely to be seen by a nephrologist, receive home dialysis, or receive a transplant, which makes the upward adjustment in kidney function more concerning as it can delay delivery of care. So when you think about this race adjustment happening for two decades in the U.S., the number of people potentially affected is huge. What happens to all these patients and their care?”
Based on the study’s preliminary findings, the MGB hospital system eliminated the use of race adjusted eGFR in June 2020. At the time, only a few other health systems in the U.S. had taken this action.
The unscientific use of race in medicine
“The concept of race has no genetic or scientific basis.”
– J. Craig Venter, the Human Genome Project, June 2000
More than 20 years after the completion of the first draft of the human genome, race-biased algorithms such as eGFR persist in healthcare across many disciplines.
“We have 10 more race adjustments I’m trying to address across our system,” says Tom Sequist, MD, MPH, Brigham internist and chief patient experience and equity officer for Mass General Brigham. “The challenges for dealing with them are all different. But they all face two common barriers: inertia and resistance to change.”
Sequist adds that race adjustments stretch beyond the realm of the hospital or the electronic medical record.
“An outside testing lab might have a racial algorithm built in,” he says. “Or equipment for a cardiac test may require the clinician enter the patient’s race, and the patient might never know.”
Another flaw is that many race adjustments classify patients using an inappropriate binary distinction of Black or not Black, as in the eGFR. And none of these calculators account for the multiracial diversity of our population.
“The American College of Cardiology has an online risk estimator for ASCVD [atherosclerotic cardiovascular disease] with required race categories of white, African American, and Other,” says Sequist. “But the results for Other are identical to the results for white, so you have an illusion of a nonbinary race choice between Black and not Black. On top of which, what do you enter if a patient self-identifies as both Black and white?”
One of these is not like the others
Age, height, weight, sex, and race are common clinical variables collected by physicians and researchers. They drive everything from prescribing decisions to diagnostic decision trees to treatment plans to research and trial protocols. Yet, among those, race is the only variable with neither a biological component nor universal criteria to describe it.
“We know race isn’t biological,” Sequist says, shaking his head. “But we’ve been treating it that way for years! And even more problematic is that we don’t have a consistent way for collecting race data. When we see race data in Epic (the Brigham’s electronic medical record system), we don’t know whether the patient self-identified, if a clinician or registration staff made an assumption, what the choices were when it was entered, or whether the patient even knows what was entered.”
Another complication with race as a standalone medical demographic is that, unlike ancestry or ethnicity, it is often dependent on geography, history, or who is making the assessment. A person considered white in the Bahamas or Brazil may be considered Black in the U.S. A person who has identified as Black their entire life may, after death, be described as white by a physician or medical examiner filling out a death certificate.
Throughout U.S. history, states had different rules for defining racial groups, and the rules varied depending on the race. Native Americans could be white if they had one white parent. In one state, a person was Black if they had a Black parent. In another state, they were Black if they had a Black grandparent. By the 20th century, Jim Crow laws cemented the infamous “one-drop rule,” where anyone with one drop of African ancestry was defined as Black.
“We are the only country in the world that applies the one-drop rule, and the only group that the one-drop rule applies to is people of African descent,” says G. Reginald Daniel, professor of sociology at the University of California, Santa Barbara.1

Health—and healthcare—mirror society
“Race is not a biological category that naturally produces health disparities because of genetic differences. Race is a political category that has staggering biological consequences because of the impact of social inequality on people’s health.”
– Dorothy Roberts, “Fatal Invention: How Science, Politics, and Big Business Re-create Race in the Twenty-First Century,” p. 129
For centuries, structural racism in the U.S. has created and perpetuated racial and ethnic disparities in health, housing, employment, access to healthy food, and proximity to environmental hazards (often referred to as social determinants of health). This same racism then blames disadvantaged groups for those disparities, due to imagined genetic, biological, character, or behavioral defects.
“We’ve had a decade of genome-wide association studies now, we’ve spent billions and billions of dollars…it looks like 97% of the mortality disparity between blacks and whites in the United States has nothing to do with genes,” says McGill University epidemiologist Jay Kaufman in Angela Saini’s 2019 book, “Superior: The Return of Race Science.”
If racial health disparities are a reflection, even a measure, of structural racism, what is a new way forward?
As widely documented, the COVID-19 pandemic disproportionately devastated minority communities. The Brigham’s multifaceted response to the crisis hinged on gathering richer demographic information related to social determinants of health: race, ethnicity, language, sex, insurance status, and geographic location.
In July 2020, a group of Brigham faculty discussed the benefits of expanded demographic data gathering in a Harvard Business Review article, “A Data-Driven Approach to Addressing Racial Disparities in Healthcare Outcomes”: This powerful and underused approach revealed inequities that otherwise would have remained hidden. For example, we found that Hispanic non-English speaking patients were dying at higher rates than Hispanic English-speaking patients. Further risk-adjustment analyses then confirmed the finding and led to quality-improvement efforts to improve patient access to language interpreters.2
While gathering more expansive demographic data helps reveal disparities across many aspects of healthcare, data is not the only answer, especially when it is easily misinterpreted.
“Interpreting data with a health equity lens is essential,” says Zara Cooper, MD, MSc, an acute care surgeon and co-chair of the Brigham Health Board of Trustees Committee for Diversity, Equity, Inclusion and Community Health. “Our goal is to infuse equity in everything we do. When we can better understand the experience of our patients and our employees, we can better align our intentions and performance with our values.”
Key to this effort at the Brigham has been looking at health equity as a quality and safety issue, not just in outcomes of care but in access to care itself.
Better data, better care
“If medicine is to fulfill her great task, then she must enter the political and social life. Do we not always find the diseases of the populace traceable to defects in society?”
– Rudolf Virchow, German physician and pathologist, 1848
“Our goal is to think about equity up front, as integral to safety,” says Andrew Resnick, former senior vice president and chief quality and safety officer at the Brigham. “And our approach is based on the evidence that when we can make care better for people facing the biggest barriers, we make it better for everyone.”
This involves evaluating and considering richer demographic data across the spectrum and reporting it on dashboards in every clinical area.
“In the old days, we avoided demographics,” says Resnick. “Now, we know demographics can help us understand how equity contributes to problems. We ask a lot of what-if questions in every case review.”
Resnick cites two scenarios to demonstrate how collecting more robust demographic data reveals inequities that might otherwise go undetected.
• Scenario 1: “60-year-old woman has trouble getting her medication at the pharmacy.”
• Scenario 2: “60-year-old non-English-speaking woman from the Dominican Republic with low vision has trouble getting her medication at the pharmacy.”
“Assessing equity up front for all cases enables us to identify corrective actions that promote equity and safety in everything we do,” says Resnick. “We can’t correct problems we don’t know about. And the bottom line is that we know there is no quality or safety without equity.”
From data to empathy
“It is not your duty to finish the work of perfecting the world, but neither are you at liberty to neglect it.”
– Rabbi Tarfon, “The Mishnah,” first century CE
“COVID-19 shattered the compartments of our lives,” says Cooper. “The crisis showed us how much this organization needs data to persuade people to act. We can’t turn everyone into an empathy expert, but we can drive home a core value and a recognition that we’re all interconnected.”
As medicine and science grapple with the long legacy of racism, the challenge of embracing more varied aspects of humanity beyond skin color is akin to the challenges of learning multiple languages.
“The story is that it’s going to take a long time,” says Cooper. “Many of us were raised to think that a racist is a person, without recognizing that society is set up to be racist. We each have a personal responsibility for dismantling it. This is a fundamental structural change that should be forcing each one of us to rethink our society, our medicine, and our healthcare.”
On September 23, 2021, the National Kidney Foundation and the American Society of Nephrology Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease published “Unifying Approach for GFR Estimation,” including three high-priority recommendations to remove race from calculations, adopt other race-free markers such as Cystatin-C, and conduct research interventions “that promote health equity and do not generate disparate care.”3
As a member of the task force that included nephrologists, primary care providers, researchers, and most important, patients, Mendu is grateful for the progress. “Getting rid of the race multiplier is not enough, but it’s progress,” she says. “I hope we can keep cultivating an environment that empowers people who are focused on equity. There’s so much more work to be done.”
Tackling inequities in transplant wait lists
Patients’ eGFR scores are key to being placed on kidney transplant wait lists. Additionally, wait time—the amount of time one spends on a transplant wait list—is one of the most important factors in determining eligibility for a transplant.
In January 2023, the Organ Procurement and Transplantation Network (OPTN) gave all U.S. organ transplant centers one year to evaluate the eGFR scores of people on their kidney transplant wait lists and recompute them if the scores had used the race-based eGFR modifier.
The goal of the OPTN’s new mandate is to improve transplant equity by backdating the wait times of Black kidney transplant candidates disadvantaged by the race-based eGFR modifier, which inflated their kidney function scores by as much as 20%.
“If a patient had wait list time prolonged because the race multiplier inflated their estimated kidney function, they are going to get their wait list time adjusted,” says Mendu, now an associate chief medical officer and vice president of medical affairs at the Brigham.
Mendu notes that moving to the race-free eGFR equations is one element in a broader strategy to bring equity to patients with kidney disease. Black people in the U.S. are nearly four times as likely to be diagnosed with kidney failure as white people. However, only 30% of the people currently on the kidney transplant wait list are Black.
“We can adopt race-free eGFR equations, but we need to address underlying structures of improving patients’ access to specialists and getting on the transplant wait list,” says Mendu. “We collectively have a lot of work to do to ensure equity for people with kidney disease.”
A different biomarker
Mendu is also studying whether cystatin C, another kidney function biomarker, will provide a clearer view of kidney function.
“As one of the first large institutions to move away from eGFR, we’ve been using cystatin C for several years,” says Mendu. “With cystatin C, about one-third of our patients with chronic kidney disease were reclassified, and we didn’t observe differences based on race, which is good. Cystatin C offers an opportunity to better understand a patient’s kidney function.”
Meanwhile, Mendu continues to investigate how the Brigham’s 2020 conversion to using cystatin C has influenced patient care.
“We’re looking at whether the change improved transplantation rates for previously disadvantaged patients or if their medications changed as a result,” says Mendu. “We’re also looking for any unintended consequences.”
Even as she works to eliminate race-based medicine, Mendu stays focused on broader issues of equity for the millions of people across the country who have CKD.
“At the end of the day, the wait for a kidney transplant often takes years,” says Mendu. “We know there are significant racial and economic disparities in wait times. We need to consider all opportunities to improve the status quo.”
Epilogue
On September 16, 2020, Audrey repeated her annual task of logging into her patient portal to see the test results from her annual physical. The race adjustment for eGFR was gone.
She was relieved. In the years since 2012, she did extensive research and reading to understand more about the history of racism in science and medicine, and what the Brigham is doing to identify and eradicate it. She used what she learned to write this story.
SOURCES
1 Wright L, “One Drop of Blood,” The New Yorker. July 24, 1994.
2 Sivashanker K, Duong T, Ford S, Clark C, Eappen S. “A Data-Driven Approach to Addressing Racial Disparities in Health Care Outcomes,” Harvard Business Review. July 21, 2020.
3Delgado C, Baweja M, Crews D C, et al. “A Unifying Approach for GFR Estimation: Recommendations of the NKFASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease,” American Journal of Kidney Diseases, 2021.