When the virus arrived in the United States, some people downplayed the threat, dismissing it as ordinary influenza. Others labeled it a sham, a hoax. Conspiracy theories abounded.
People argued over masks, widespread shutdowns, and other precautions. In the absence of reliable treatments and natural or vaccine-acquired immunity, misinformation thrived. So-called cures circulated that ranged from ineffective to life-threatening. The year was 1918. And the pandemic was a strain of H1N1 influenza that ravaged the globe. By the time the pandemic ended in 1920, more than 500 million people—a third of the worldwide population—were infected, and at least 50 million died.
Today, as the world continues to grapple with the unprecedented COVID-19 pandemic, we seek answers from science and history and encounter old stumbling blocks.
BLINDED BY SUCCESS
“One hundred years ago, measles, diphtheria, or pertussis would’ve been among the top 10 causes of morbidity and death,” says Lindsey Baden, MD, director of clinical research in the Brigham’s Division of Infectious Disease. “We would have smallpox every day here, but because of the vaccine, we don’t. That’s the problem with vaccines: They’re so good. How do you say ‘thank you’ for stopping a bad thing from happening?”
When society forgets vaccines are responsible for eradicating diseases like smallpox and measles, Baden notes, that amnesia contributes to science resistance. The anti-vax movement is a prominent example, with campaigns of misinformation and disinformation blaming vaccines for causing autism or other harms.
Among some people, anti-vaxxing philosophies, false notions that the COVID-19 pandemic is a hoax, and perceived loss of freedom during stay-home advisories have fomented suspicion and disbelief. As a result, people around the globe are beset by multiple contagions: a virus new to humans, the spread of misinformation, and distrust of science. Each contagion requires a collective, multilayered approach for containing its deadly spread.
AS STRONG AS SWISS CHEESE
Countries that have contained COVID-19 have deployed multiple tools: vigilant and pervasive testing, contact tracing, isolating those who are sick, quarantining those who have been exposed, physically distancing, wearing masks, increasing hygiene practices such as handwashing and covering coughs and sneezes, avoiding crowded areas—especially indoors—and improving indoor ventilation.
None of these protections is foolproof on its own. But scientific evidence repeatedly shows combining these interventions can be remarkably effective at containing the spread of highly contagious respiratory diseases such as COVID-19.
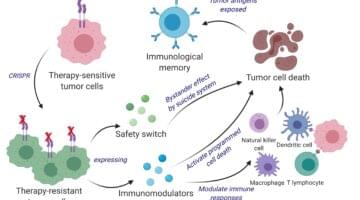
Scientists call this the “Swiss-cheese model,” where each safeguard is like a slice of Swiss cheese, where the holes represent a weakness in the intervention. When used together consistently, the weaknesses in any single layer of protection can be offset by the strengths of other layers of intervention (see Figure 1). And the more interventions are combined, the more successfully contagion can be contained.
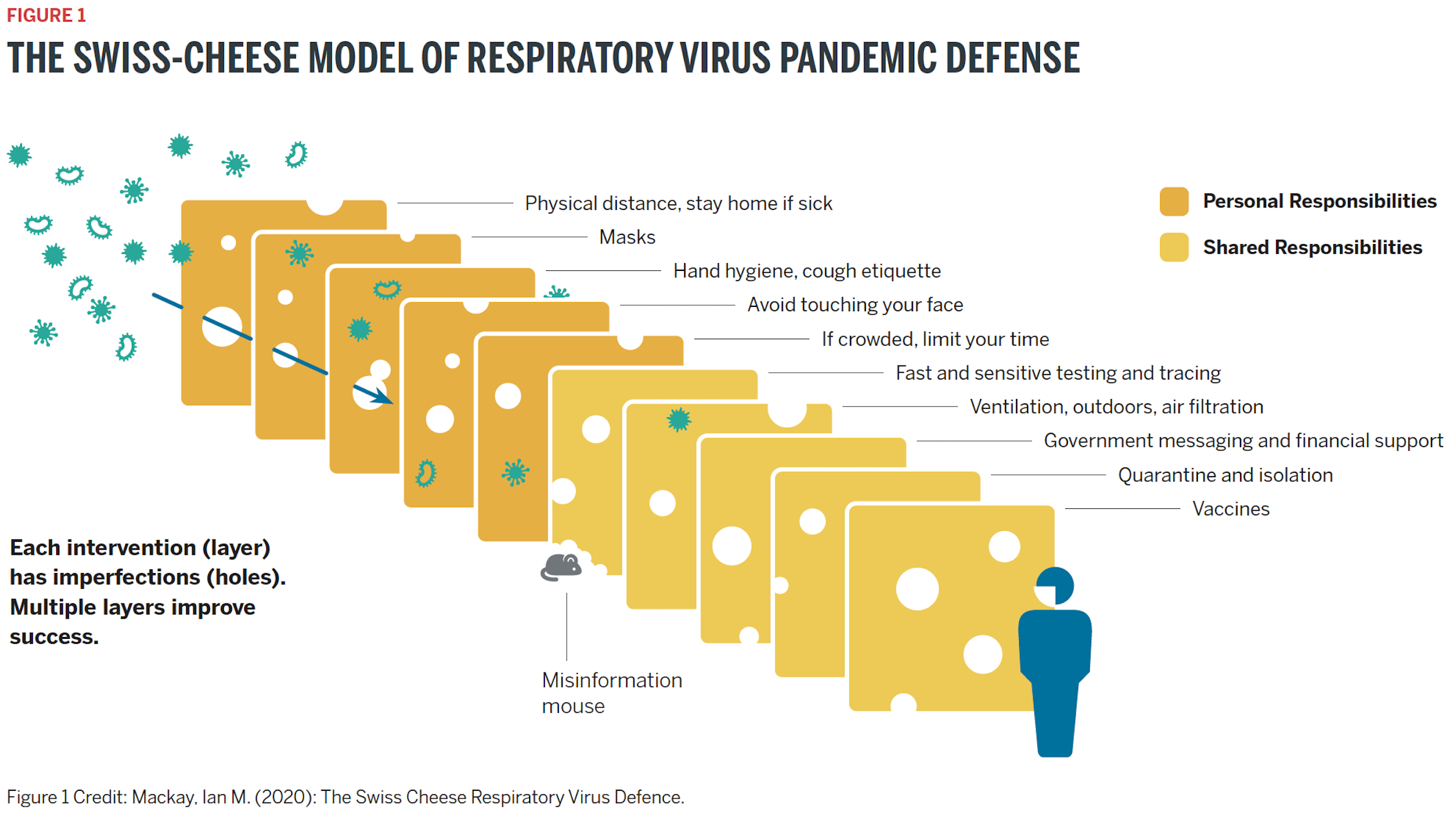
In this Swiss cheese model, the “misinformation mouse” in the middle of the diagram is chewing a new hole in a slice of cheese. This illustrates how false information, such as widely discredited notions that masks make people sick or that vaccines are more harmful than the diseases they prevent, can weaken the effectiveness of any intervention.

THE CASE FOR MASKS
An essential tenet of science—the only certainty is uncertainty—has held true for even the most basic public health guidelines around COVID-19. Today, scientific evidence abounds for the effectiveness of masks at reducing transmissions of COVID-19. But early in the COVID-19 pandemic, experts were skeptical of their use—a moment reluctant mask wearers and mask refusers have fixed on.
Michael Klompas, MD, an infectious disease specialist and hospital epidemiologist, leads the Brigham’s Infection Control team. He explains experts’ initial skepticism on the effectiveness of masks was based on historical studies of masking in households and dormitories to prevent influenza.
This aspect of influenza and SARS-CoV-2 is starkly different from SARS-CoV-1, the coronavirus that causes severe acute respiratory syndrome (SARS), which struck China, Toronto, and other locations around the world in 2003.
“With the SARS situation in 2003, it was much easier to identify who was ill and isolate people who were identifiably sick,” says Klompas. “People who weren’t sick with SARS were much less likely to transmit the virus, so it was not so important for all asymptomatic people to wear masks all the time. But COVID-19 is very different. Many people who either don’t have symptoms or don’t have them yet can transmit SARS-CoV-2. So, we adapted.”
The fact that an infected individual can have zero symptoms and still be contagious explains why COVID-19 is so successful at infecting so many people. In fact, Klompas says, the asymptomatic and presymptomatic periods two days before symptoms are the highest risk periods for transmission.
“People can feel perfectly well and go out and about, and not recognize they are infected and could be infecting others,” says Klompas. “That’s why physical distancing and pre-emptive masking are so important. They help protect us when interacting with people who appear to be perfectly well but who might be highly contagious.”

RESPECTING THE VIRUS—AND EACH OTHER
Eager to learn the true value of the many infection control measures that the Brigham institutes against COVID-19, Klompas and his colleagues studied the rate of hospital-acquired COVID-19. The team analyzed all cases in which patients tested positive for COVID-19 three days or later after coming to the hospital and up to 14 days after discharge. The data showed the rate of hospital-acquired infections was near zero.
The Brigham maintained near zero-transmission levels for months, until a cluster of dozens of cases was identified in late September and early October. The hospital’s Infection Control team contained the cluster within two weeks by applying many of the interventions shown in the cheese chart in Figure 1: increased testing of employees and inpatients regardless of symptoms, robust contact tracing, re-emphasizing physical distancing and use of protective gear such as masks and eye protection, and genomic analysis of positive cases.
Even with this incident, the prevalence rate of positive cases at the hospital was 0.1%—less than half of the city’s and state’s rates at the time. Skyrocketing cases across the U.S. in recent months further underscore how ongoing infection control demands patience, vigilance, and understanding.
“When it comes to COVID-19, it’s about respect,” Klompas says. “Respect the virus and its capacity to transmit and defy our best intentions. Respect people, their fears and vulnerabilities, and the virus’s disproportionate impact on certain populations.”

TESTING, TREATING, TRACING
One of the ways COVID-19 has defied best intentions is by obscuring who is contagious. Initial attempts to contain the pandemic limited diagnostic testing to symptomatic people, and test results could take as long as 10 days.
While scientists eventually learned the virus spreads as much from asymptomatic and presymptomatic people, testing criteria still favor people with COVID-19 symptoms. Asymptomatic and presymptomatic people continue to face barriers to testing, in part due to the expense and time-intensive, lab-based process of the diagnostic PCR test, which identifies active infection at the molecular level.
Scientists are increasingly advocating using cheaper, faster antigen tests to identify infectious people regardless of their symptoms. Epidemiologist Michael Mina, MD, argues if people could rapidly test themselves at home daily, or nearly daily, they could make better decisions in their work and social lives.
“I think a new era of massively distributed at-home rapid tests is our best hope to limit spread without massive lockdowns,” Mina tweeted on November 3. “We should push for these so we can bring outbreaks under control and return to a semblance of normalcy as soon as we can—before vaccines.”
One project—TestBoston—is exploring how large-scale distribution of at-home test kits could help contain COVID-19. Led by infectious disease specialists Lisa Cosimi, MD, Deborah Hung, MD, PhD, and Ann Woolley, MD, MPH, TestBoston is a research collaboration of the Brigham and the Broad Institute of Harvard and MIT. The project delivers free, monthly, at-home testing kits to 10,000 individuals in the Greater Boston area for six months.
“With TestBoston, we want to make testing more accessible, especially for people who have been disproportionately impacted by COVID-19,” says Woolley.
Participants return their test kits to the Broad and receive results within 24 hours. The study team hopes this system can help curb outbreaks by reducing delays in care for patients who test positive and enabling faster contact tracing.
Though TestBoston surpasses general testing today, Cosimi says, “Ideally, we’d push this even further, so people could access rapid testing that provides results in minutes instead of a day and test more frequently than monthly.”
One of the biggest arguments against rapid antigen tests concerns accuracy. Compared with the gold-standard PCR tests, which are sensitive enough to produce accurate results up to 98% of the time, current antigen tests have an 84% to 97% sensitivity rate. And judging tests’ accuracy is complicated by their different rates of false positives and false negatives. Despite this complexity, Mina and Cosimi both advise that, when it comes to testing, perfect is the enemy of the good.
“In this pandemic, it’s essential to know who is the most contagious,” says Cosimi. “A less sensitive rapid test conducted more frequently may have a better chance of capturing those people. This could give us a better chance to provide early treatment that keeps infected people out of the hospital and conduct more timely contact tracing to better contain the spread.”
BOOSTING TRUST IN VACCINES
As COVID-19 cases spiraled out of control across the U.S. in November, the global race to produce vaccines for COVID-19 provoked great anticipation—and anxiety.
“The great thing about the vaccine effort is that it has proceeded at an extraordinarily fast pace, and it’s exciting that some of my colleagues at the Brigham have been at the forefront of that effort,” says infectious disease specialist Paul Sax, MD.
“One of the most important features of any vaccine is that it be safe, because we don’t want a vaccine not accepted by the public,” he says. “There’s already a vocal distrust of vaccines, and we need strong efficacy and safety data to reassure the public.”
At the Brigham, researchers led by Baden enrolled patients in the nation’s first phase 3 trial of a COVID-19 vaccine candidate. Initial trial data generated from 30,000 individuals across the U.S. identified no safety concerns to date about the vaccine. Baden says understanding how the vaccine is tolerated in 15,000 study volunteers allows researchers to define what the side effect profile may be when they move to vaccinate millions.
“The vaccine candidate itself does not contain live virus—it’s an mRNA construct,” Baden explains. “Participants may contract or be exposed to COVID-19 through interactions in the community. Our hope is that the vaccine will decrease risk of acquiring COVID-19 from normal work or community interactions, or that the vaccine will decrease severity of symptoms and contagiousness.”
As knowledge advances through the trial, he adds, “and we determine what works or what doesn’t, we will stop doing what doesn’t work and figure out how to deploy what does. Then, we need to consider how we act equitably to distribute a vaccine across society.”
On December 15, FDA scientists confirmed the vaccine’s safety, with an efficacy rate of 94.1%. Two days later, the FDA approved the vaccine for emergency use.

PROTECTION FOR ALL
Once a vaccine is widely available and embraced, it could lead to the ideal solution to many infectious diseases: herd immunity. This is when populations—the herd—become immune to a particular infectious disease without being infected first. When more than 70% to 90% of a population has been exposed to an infection or vaccinated against it, herd immunity slows or stops an infectious disease’s ability to spread.
Discussions of herd immunity for COVID-19 have caused some confusion. As more people become infected with the virus, some have wondered if herd immunity could be achieved without a vaccine.
Sax adds, “In the 21st century, with access to so much scientific knowledge and innovation, most infectious disease specialists agree that herd immunity is a result of robust public health policies. It is not, by itself, an ethical or responsible strategy for containing pandemics.”
Achieving and maintaining herd immunity is an ongoing effort, which can backslide when vaccines aren’t used. This has happened with measles, a highly contagious viral infection that can cause serious complications in small children. Declared eliminated by the U.S. Centers for Disease Control and Prevention in 2000 thanks to widespread global vaccinations, measles resurged when vaccine skeptics did not inoculate their children against it. In 2019 alone, the U.S. saw 1,282 measles cases—the largest number in one calendar year since 1992. Worldwide, measles deaths increased 50% between 2016 and 2019.
Baden says the promise of herd immunity through vaccination should be an incentive and reminder to society about why vaccines matter.
“Getting vaccinated benefits not just you, but those around you, particularly those who may be vulnerable—like immunocompromised individuals undergoing cancer treatment, or those who are pregnant, or the elderly, or babies,” Baden explains.
SEEING THE LIGHT
In the midst of so many crises, from the virus itself to the social upheaval, misinformation, and distrust generated in its wake, optimism can be hard to come by. But of all the things uniting scientists of the front lines of this pandemic, optimism is one of their strongest bonds.
“There is a light at the end of the tunnel,” Kuritzkes says. “We’ve learned how to protect people from this disease, and we all need to keep at it. There’s reason to be optimistic while we carefully monitor the situation and prepare to put out small fires as they emerge.”
When everyone follows the science, commits to best practices, and shares responsibility for keeping each other safe, COVID-19 can be contained. To get there sooner, heed the experts’ advice:
“Protect yourself by wearing a mask, washing your hands, and physical distancing,” Kuritzkes says. “If we keep doing that, there’s reason to expect that by late 2021, we will be in a better position than we are today.”