For researchers who study mental health disorders, the heat is on to discover their root biological causes and develop new treatment strategies and targets.
“These illnesses are not like tumors and strokes that you can see on a scan—yet,” says David Silbersweig, MD, chair of the Department of Psychiatry at the Brigham. “Recent developments in brain imaging and other technologies are helping us gain traction. Many of our faculty and trainees are involved in research to identify the pathophysiology of mental illness.”
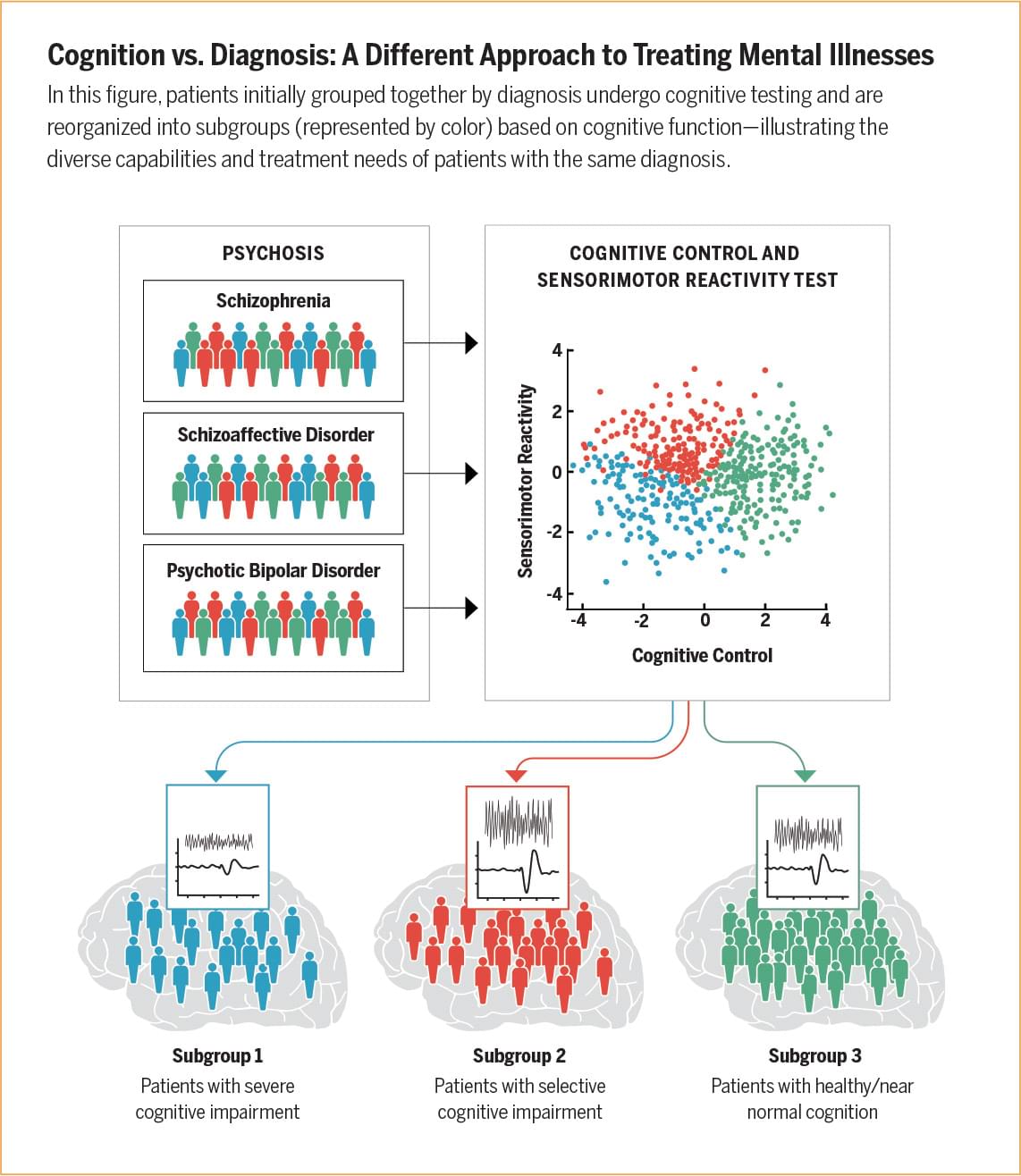
Brigham researchers are working to decipher the root causes of mental illness using advanced imaging techniques, genomic research, and analysis of big data to yield a more precise understanding of the biology and physiology of these disorders.
Kate Burdick, PhD, is one of dozens of psychiatric investigators at the Brigham. As director of the Brigham’s Mood and Psychosis Research Program, she and her team study cognitive changes in people who have bipolar disorder, major depressive disorder, and schizophrenia.
“We’re finding that cognitive decline is closely tied to the number of manic-depressive episodes people experience over their lifetimes,” Burdick says. “Two people can be diagnosed with bipolar disorder and have it for 20 years, but the one who’s had two major episodes will have better cognitive function than the other who’s had 20 episodes in that time.”
After isolating data from patients with the most severe forms of the illness, Burdick’s lab found more genetic risk factors and history of childhood trauma in that group than in people who have had fewer manic-depressive episodes.
“We need to think about cognition as a treatment target, instead of focusing solely on primary mood symptoms,” she says. “Cognitive decline is the number one predictor of disability in these diseases. We’re starting to ask why manic-depressive episodes trigger an inflammatory response in the brain and cause these hits to cognition. Maybe if we target those triggers, we can stop the worst-case trajectories of these disorders.”
Some of the Brigham’s newest evidence-based psychiatric treatments include brain stimulation and intravenous ketamine infusions. Though not yet covered by insurance, these approaches are showing promising results for some patients who don’t experience enough relief from traditional psychiatric medications or therapies.