Now more than ever, good heart health can save your life.
In addition to being the leading cause of death for adults worldwide, heart disease is a major risk factor for suffering serious illness from COVID-19. Research is also revealing the virus can inflict lasting damage on the heart, even for people with no prior history of heart problems.
But experts maintain there are still plenty of ways to take charge and prevent heart issues from worsening or emerging at all. In fact, with lifestyle changes, medications, or a combination of strategies, at least 80% of heart diseases can be prevented. Cardiovascular leaders have also seen patients and doctors embrace telehealth as a way to manage chronic conditions while physically distancing, a paradigm shift that has become a shining example of how the field has innovated through adversity.
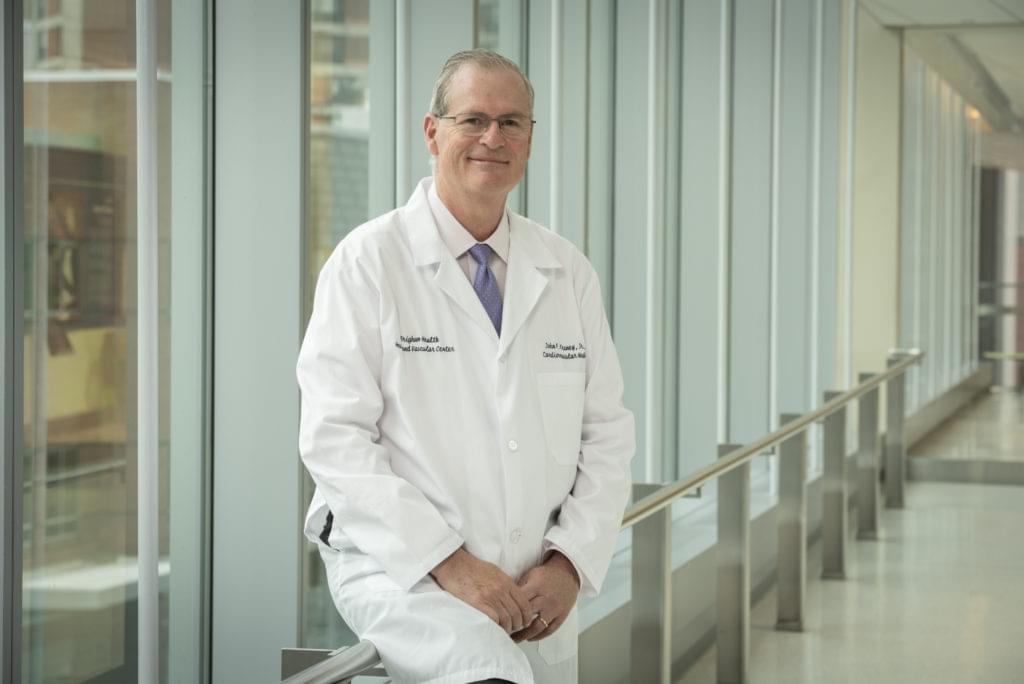
The Brigham’s pioneering cardiologists invented ways to intervene during and after cardiac catastrophes. As COVID-19 deals one of the toughest stress tests on the heart and on our healthcare systems, they are devising new and expanded approaches to help people reduce their cardiac risk—in the hospital, at home, and in the future.
DESTABILIZING FORCES
In a typical month, 5,000 people journey to Boston seeking expert cardiovascular care at the Brigham, a place steeped in firsts and bests in the field.
However, March 2020 was anything but typical. During the third week of March, 95% of scheduled elective (non-emergency) heart procedures and visits came to a stop in order to convert the Brigham’s Shapiro Cardiovascular Center for the exclusive care of patients with COVID-19.
It was also a time when most ongoing research paused and investigators quickly shifted gears to study COVID-19. Faced with an unknown disease, many clinicians and scientists were initially surprised by the cardiac complications unleashed by COVID-19, which at first glance seemed to mainly affect the respiratory system.
For decades, Libby and Ridker have studied the role of inflammation in heart disease, including how an inflammatory response to a virus can either protect the body or make it vulnerable to worst-case scenarios—including heart damage.
“It’s like one big stress test of the heart,” said Ridker in an April report from Harvard Medical School.
For example, in response to the infection, the liver produces defensive proteins that can make blood more prone to clotting and also reduce the body’s ability to make natural clot-dissolving substances. Those clots can clog small blood vessels in the heart and other organs, restrict oxygen and nutrients, and cause multiple organs to fail.

Reports from the U.S. Centers for Disease Control and Prevention (CDC) confirmed the link between the virus and heart complications. In June 2020, the CDC released a surveillance study of more than 1.3 million positive U.S. cases of COVID-19 showing 14% of patients were hospitalized, 2% required ICU care, and 5% died. Heart disease was the most common underlying condition reported, making people six times more likely to be hospitalized and 12 times more likely to die from the virus.
After months of study, Libby wrote in the European Heart Journal that COVID-19 could be considered an endothelial disease, because of the way the virus affects the inner cellular lining of the blood vessels (the arteries, veins, and capillaries) and the lymphatic system.
“This unifying hypothesis can help to understand the complex pathophysiology of this current plague and may also help to inform our therapeutic approaches to combatting the consequences of SARS-CoV-2 infection,” Libby concluded.
SURVEYING THE DAMAGE
In the Cardiac ICU, Erin A. Bohula, MD, DPhil, has seen the worst of COVID-19. While the initial, predominant symptoms involved the lungs, she and her team began to see the heart was affected, too—and scrambled to figure out how to stop the damage.
“We’ve seen acute cardiac injury, heart failure, cardiogenic shock, arrhythmias, and a high rate of blood clots,” says Bohula, a critical care cardiologist. “With no experience to guide us as far as what the normal course of these severe COVID manifestations is, it was a challenge to determine appropriate treatment.”
Bohula explains that the COVID-19 virus enters human host cells when the spike receptor proteins on the virus cells interact with ACE-2 receptors, which are found in the lungs, heart, kidney, and GI tract.
“That’s why we think we are seeing cytotoxic effects in those organs, including acute respiratory syndrome, acute liver injury, and acute kidney injury,” she says.
The complex problem solving required to care for patients with COVID-19 is typical for a normal day in the ICU, Bohula adds. But the unpredictable nature of the virus has been utterly confounding. While cardiac COVID complications generally predict bad outcomes for patients, survival rates differ widely. Bohula has seen several patients suffer the worst and recover.
One patient in his 80s developed severe COVID-associated pneumonia and heart dysfunction and was placed on a ventilator. With the right combination of medications and three weeks of critical care, his condition improved and he was taken off the ventilator. At four weeks, he stabilized and was discharged from the hospital.
“I was worried for him when he arrived in the ICU because of his age and the shape he was in,” she recalls. “It was amazing to see him make such a wonderful recovery. And what’s even better is that we’ve seen several people with similar or worse cases beat the odds, too.”
To advance care for critically ill patients, Bohula launched a clinical trial of anticoagulants to treat severe COVID-19. Her colleague, cardiovascular specialist and researcher Gregory Piazza, MD, MS, is studying whether low-dose anticoagulants can help patients with COVID-19 who are at increased risk for blood clots.
“We have to make sure patients who are not hospitalized for the virus but are at risk for blood clots are protected,” says Piazza, who is also leading an observational study of cardiovascular complications using data from healthcare systems nationwide.
“I think it’s going to be our biggest contribution to this fight: to understand what the cardiac complications of this disease will be in the future,” Piazza adds. “What will the cardiovascular landscape look like in the aftermath of COVID-19? These are things we will need to learn over the next months and years. We expect we are going to have to provide a greater level of care to patients who have been affected by this.”
ROLLING WITH THE CHANGES
As the crisis transformed the hospital, a positive paradigm shift emerged to help doctors stay in touch with patients following governmental stay-at-home advisories. Prior to the shutdown, telehealth accounted for just 1% of all cardiovascular visits at the Brigham. By late March, two weeks into the shutdown, 96% of patient visits were held by phone or videoconference.
Piazza says the accessibility and frequent touchpoints of virtual visits are especially advantageous for frail and elderly patients, who may have trouble arranging transportation and navigating the hospital even in normal circumstances.
“Once we were better connected virtually, we were reaching patients quickly and effectively, which meant we were able to ward off complications that would have resulted in a hospital visit,” says Piazza. “Plus the added convenience brings better adherence to a follow-up plan, which could improve outcomes.”
Before the pandemic, Piazza says it wasn’t unusual for 10% of patients to miss their office appointments in a given week, which is a typical no-show range for specialist clinics.
“I haven’t had a single no-show for virtual visits,” he says. “Patients want to be able to interact with their providers. They are prepared for their virtual visits, and we are able to provide a high level of care using these tools.”
Piazza adds, “Virtual visits can’t replace the element of human touch, but they have certainly extended the reach of our care. As a physician, I embrace the change.”
A SMARTER HEART
While the move to telehealth was a radical departure for most of the division, virtual care was already the rule, not the exception, for its offshoot Cardiovascular Medicine (CV) Innovation.
For three years, CV Innovation has been home to a groundbreaking program that helps patients track and manage high blood pressure and high cholesterol from home. More than 7,000 patients enrolled in the program use cellular or Bluetooth-enabled devices, like a blood pressure cuff for those with high blood pressure, to capture and record their stats every day. The data transmits to their electronic health records at the Brigham.
What pushes CV Innovation’s remote monitoring program beyond most telehealth practices is its use of artificial intelligence. The program is powered by an algorithm developed by top Brigham cardiologists and hypertension specialists, which tracks and analyzes patients’ data in real time to ensure treatments are effective and appropriate for each individual’s needs.
Early results have been promising. In traditional office-based care, only 50% of people with hypertension have it under control. During the pilot study of the remote program, 91% of patients who stuck with the program reached their blood pressure goals after about eight weeks.
“As cardiologists, we may see a patient once every six months, and we can be so busy in between that we generally don’t know what’s going on in patients’ lives to prevent them from reaching their goals,” says Christopher P. Cannon, MD, a cardiologist and director of education in CV Innovation. “In CV Innovation, we identify those patients who are not at goal and monitor and adjust their treatment by constantly engaging and supporting them.”

CONSTANT CONTACT
In December 2019, Robert Ross had undergone an aortic valve replacement at the Brigham. As part of his aftercare, his cardiologist recommended he enroll in CV Innovation’s remote monitoring program to keep a watch on his blood pressure from home.
“After the surgery, I needed to have my blood pressure checked twice a day—and it would have been impossible to go to my doctor’s office for all of those checks,” Ross says. “I knew how much could be achieved just by having the right tools and good communication. With a phone and the blood pressure cuff, I felt confident that I could handle it and be supported.”
If Ross’s blood pressure readings changed significantly, the built-in algorithm would detect the change and alert his health coach, or patient navigator, to call him and check in.
Samantha “Sam” Subramaniam is a patient navigator on the CV Innovations team. Working from her home, Subramaniam maintains constant communication with Cannon and other medical advisors. She monitors patients’ data on their individual dashboards and works with them to help improve their numbers and cut their cardiac risk.
“High blood pressure and cholesterol bring patients to us, but we can help with so much more,” says Subramaniam. “We are their cheerleaders to give them that extra push to make healthy choices, and we become their healthcare liaisons when they need an expert opinion. When patients reach their goals, it’s a great moment of celebration for all of us.”
STEADY ON
CV Innovation is at the forefront of using data to prevent or mitigate chronic diseases. In addition to directly improving care for patients at the Brigham, the program is synced with a massive research enterprise called One Brave Idea, a venture between the American Heart Association, Verily Health, and the Brigham that uses big data to identify and prevent heart disease as early as possible. For now, the immediate challenge is helping people stay healthy and avoid dangerous collisions with COVID-19.
“Since cardiovascular diseases, including hypertension, are major risk factors for adverse outcomes among patients who get COVID-19, our patient population is a high-risk group,” Cannon says. “Public health officials have noted the importance of having other diseases well controlled, so this program is a great tool to have. If one of our patients gets COVID-19, they will be as healthy as possible to fight it.”
Ross is still enrolled in the remote monitoring program. Each day, he faithfully takes his blood pressure and watches the readings transmit to his dashboard, where Subramaniam and other patient navigators keep track of his progress.
“When you say telehealth or virtual medicine, it sounds impersonal—but this has been very personal and humane,” says Ross. “Talking with Sam is very focusing, since the data is all right there to see and there are no distractions like there might be in an office setting. And with everything happening, it’s reassuring to stay safe at home while taking care of my health.”
Subramaniam is excited to help more people get control of their overall health and well-being—ever more vital in a pandemic-altered world.
“I never felt like I could save a life,” Subramaniam says. “But there are moments when I feel like I have, even in a small way. I can’t wait to talk to patients, hear their stories, and help them have a healthier day. We’re not just thinking about great things we can do in the next year or decade. We’re excited to think of what we can do today.”