Millions of people in the United States have damage to their cartilage, which acts as a cushion for joints throughout the body. When this human shock absorber is injured through accidents, injuries, or general wear, it can cause painful friction between bones of the joints and loss of function.
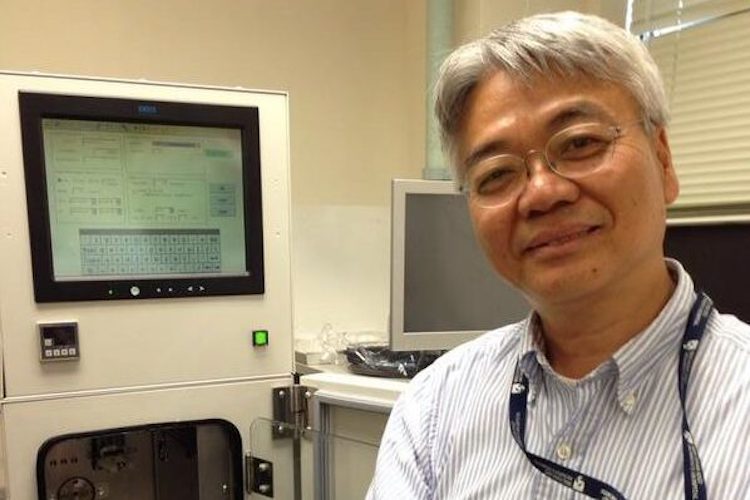
“If damaged cartilage in the knee isn’t treated, it can develop into osteoarthritis and increase the risk of requiring knee replacement surgery in the future,” says Shuichi Mizuno, PhD, who directs a laboratory in BWH’s Department of Orthopaedics.
Surgically, physicians can try to help heal cartilage in the knee by filling the cartilage defect with repair tissue. However, the quality and durability of repair tissue is poor and it is slow to naturally regenerate, which means subsequent surgeries are often needed. For the past couple decades, the recovery time after surgery has remained the same—up to one year until patients can run, play sports like basketball, or do other strenuous activities.
When Mizuno started working on a novel cell process technology that could generate cartilage tissue back in 1995, he had no idea it would take more than 20 years to see his invention become a reality. But he has persevered.
Mizuno created NeoCart® to speed up the process of growing new cartilage cells in the lab. The idea is to take a patient’s own cartilage cells from another part of the body and grow them in culture. Then, the cartilage cells are placed in the cell processor, which applies pressure similar to the inside of the knee cartilage, which is like the underwater pressure felt by a deep-sea diver.
“NeoCart® stimulates cells to think they’re in the body, with the pressure that is usually felt from walking, for example,” Mizuno says. “This causes the cells to multiply rapidly. After a few weeks, surgeons can implant a matrix of cartilage tissue that would more quickly integrate with the body, treat pain at the source, and shorten recovery time.”
Mizuno first had the idea as a doctoral student studying biomedical engineering and continued the project during postdoctoral research in biology under the guidance of internationally recognized researcher Julie Glowacki, PhD, director of BWH’s Skeletal Biology Research Laboratory.
“During the past 20 years, we’ve had so many startup companies to make this idea and the technology survive,” Mizuno says. “We’ve evolved the design, and in September 2017, we implanted the last of 249 patients in the phase 3 clinical trial. If the results are good, we’ll submit to the FDA for approval this fall.”
Mizuno has also been adapting the NeoCart® technology for two other purposes: repairing a damaged meniscus in the knee and disc in the spine. He hopes to move this research out of the lab and into clinical trials soon.