The whole art of medicine is in observation . . . but to educate the eye to see . . . takes time, and to make a beginning, to start . . . on the right path, is all you can do.
– William Osler, MD, Canadian physician (1849-1919)
Sight, knowledge, and understanding are far from synonymous. True understanding requires multiple viewpoints and repeated closer looks. Sir William Osler, MD, renowned 19th century physician and medical educator, examined thousands of patients and performed hundreds of autopsies to educate his eye and understand disease. While the term autopsy literally means “to see for oneself,” Osler’s work may have helped narrow the term to its modern meaning of examining a dead body to determine the cause of death.
Osler would likely be staggered by the array of observational tools available in the 21st century. From high-powered microscopes to three-dimensional scanning equipment, today’s imaging technologies can observe and record components of a live human body in real time, down to the molecular level. Physicians, surgeons, and scientists at Brigham and Women’s Hospital (BWH) use a wide array of imaging devices—often in combinations—to gain deeper understandings of the most intractable challenges of human health, ranging from heart disease to infertility to epilepsy and more.

A CLEARER VIEW OF THE HEART
“When I was in medical school in the 1980s, to look at the heart muscle you had to go to the pathology lab,” says Marcelo Di Carli, MD, executive director of the Cardiovascular Imaging Program at BWH. “In the last 10 years alone, we’ve seen a rapid evolution of imaging technology. Today, we can show you an incredibly detailed picture of the heart, from the characteristics of the muscle to the structure and function of its smallest blood vessels, and we can get that picture non-invasively in a minute or two.”
Di Carli’s team focuses on improving diagnoses, identifying markers of cardiovascular risk, and helping referring clinicians accurately triage patients so they can be matched with the correct services or procedures.
“Our goal is to help clinicians better manage their patients,” says Di Carli. “We want to give them a clearer understanding of the diagnosis and whether they might need to do an intervention and, if so, what kind it should be.”
One of the unique imaging challenges presented by the heart and its blood vessels is that they are always in motion. Like ultra-high-speed cameras, today’s scanning technologies clear that hurdle with improved speed and resolution.
Di Carli’s program is a national leader in using imaging tools to understand more deeply the biology, structure, functions, and diseases of the heart and vascular system.
“We now have ways to identify and evaluate small plaques in arteries with non-invasive imaging,” says Di Carli. “Current imaging technology can characterize the type of plaque in a vessel and determine whether it is likely to cause trouble or not. We used to spend hours to get this information, threading catheters and cameras into the heart and its surrounding vessels through an incision in a patient’s leg. Now we can
do this with a scan that requires no incision.”
Another area where Di Carli’s team has deepened insights into the cardiovascular system is in the microvasculature. Unlike the coronary arteries, these tiny vessels are so small and so deeply embedded in the heart tissue, they can’t be seen with conventional coronary angiography. The microvasculature branch out from the coronary arteries and regulate blood supply to the heart muscle, delivering oxygen and nutrients to cells inside the muscle.
“Coronary microvascular disease affects many patients, especially women, who have chest pain,” says Di Carli. “It used to be they’d come in, we’d do the standard catheter-based injection of dye, scan them, and find no obstruction in the coronary arteries, and assumed that there was nothing wrong with the heart. But they still had chest pain. Now we can obtain detailed quantitative information about their microvascular function by measuring blood flow, we can diagnose the severity of their disease, and we can test objectively whether their therapies are working. It’s completely changed our paradigms of diagnosis and care in this disease.”
SEEING A PATH TO NEW LIFE
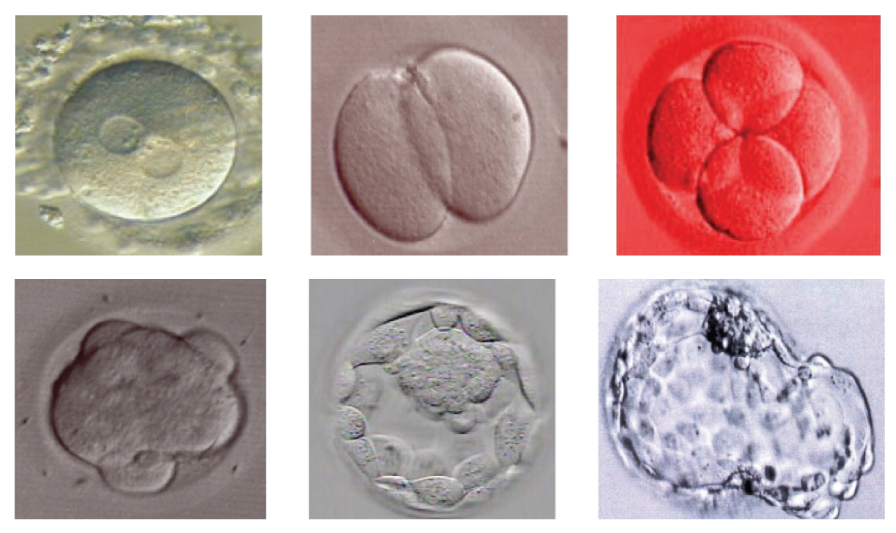
While cardiovascular imaging increasingly focuses on modern imaging technology (including ultrasound, MRI, CT, and PET), embryologists lean heavily on various types of microscopes, whose origins are ancient. The first microscopes date back more than 3,000 years and were made from globes of water-filled glass or shards of transparent crystals. Today’s high-powered microscopes enable embryologists to fertilize an egg and watch cells in an embryo divide in real time.
“After more than three decades in this field, I still get goosebumps when I see a human embryo through the microscope,” says Catherine Racowsky, PhD, director of BWH’s Assisted Reproductive Technologies Laboratory.
Racowsky’s office is crammed with photos of babies she first glimpsed as embryos. She has devoted her entire career to improving results of in vitro fertilization for women seeking to become pregnant in the face of infertility.
Nothing that is seen is seen at once in its entirety.
– Euclid of Alexandria, Greek mathematician (~325-270 BCE)
“A woman’s fertility is primarily determined by the quality of her eggs, which we know declines with increasing age, body mass index, and exposure to environmental toxins,” says Racowsky. “Aside from these factors, we still lack approaches to identify underlying mechanisms that determine egg quality. This makes it difficult to know how to reliably improve egg quality, or to predict which egg among a group of eggs will produce an embryo most likely to implant and make a baby.” Another challenge in understanding the mysteries of infertility is the quality of embryos.
“When we look at our data tracking embryo quality (by inspecting their appearance) and successful, healthy pregnancies and births, we see lower quality embryos are sometimes capable of producing healthy, full-term babies,” says Racowsky. “Clearly, visual assessment, which remains the standard approach for evaluating embryo quality, has limitations.”
The desire to help infertility patients fuels Racowsky’s quest to find new ways to observe and understand eggs and embryos at the molecular level. One possible avenue is using advanced microscopy to study mitochondria, the organelles inside cells that produce energy.
With two colleagues, Racowsky recently received a grant from the National Institutes of Health to use fluorescence lifetime imaging microscopy and genetic sequencing to observe and study mitochondrial function in eggs and embryos. Harvard University’s Dan Needleman, PhD, heads an imaging lab that uses fluorescent labeling to observe changes in mitochondria. Dagan Wells, PhD, of the University of Oxford, is a leader in pre-implantation genetic diagnostics. Working together, Racowsky, Needleman, and Wells hope these new ways of studying eggs and embryos will help them decipher whether mitochondrial activity can be a quantifiable predictor of egg and embryo quality.
“I think it’s unlikely we’ll ever have just one test for evaluating embryos,” says Racowsky. “There is so much heterogeneity among embryos and numerous possibilities to evaluate their quality. I suspect we’ll end up with a three- or four-prong approach, one of which may be the imaging technology we are currently investigating. It’s a very exciting time. There’s still so much to learn.”

MAPPING A BETTER FUTURE FOR PREEMIES
Once a woman is pregnant, the focus turns to healthy pregnancy and childbirth. Full-term pregnancy is 40 weeks. In the United States, about 1 in 10 babies is born preterm or prematurely, before the 37th week of pregnancy. While extremely preterm infants born between 22 and 28 weeks face the longest odds for surviving and thriving, all preterm infants have an increased risk for brain injuries resulting in cerebral palsy, motor problems, or cognitive delays.
For years, neuroscientists evaluated brain injury and impairment in adults by comparing healthy brain scans with scans of people with traumatic brain injuries, stroke, or diseases such as Alzheimer’s or Parkinson’s. Building a similar body of knowledge to transform care for infants and children with brain injuries is a top priority for Terrie Inder, MD, MBChB, chair of BWH’s Department of Pediatric Newborn Medicine.
It is a terrible thing to see and have no vision.
- Helen Keller, American author (1880-1968)
“We did a study across the United States to see what kinds of brain studies were done on babies who came to doctors or hospitals either comatose or stuperous or having active seizures,” says Inder. “The first thing we found was, of 4,000 babies in our study, 15 percent never had their brains looked at with any kind of scan. If you’re an adult who comes to the doctor or Emergency Department with the same symptoms, what are the chances they don’t look at your brain? Zero. But with babies, for some reason, you find more of a wait-and-see attitude. People don’t want to look.”
Inder is working to shift away from this passive approach. For nearly 20 years, she has been using magnetic resonance imaging (MRI) brain scans to identify and quantify brain injuries in premature babies, with a goal of improving their short- and long-term outcomes.
“Being able to define the presence of brain injury in babies when they go home from the hospital is critically important in terms of helping their parents understand their babies’ future risk for challenges,” Inder says. “The term commonly used in the field is ‘early intervention,’ but it’s not intervention if you’ve sustained a brain injury—it’s rehabilitation. Rehabilitation for babies with brain injuries requires the same services as for adults: occupational therapy, physical therapy, and speech therapy. Babies can respond to therapies that teach them how to suck or to coo.”
Complicating matters, getting an MRI of an infant brain requires customizing standard scanning equipment and its supporting software, which are built for adults. Inder has partnered with colleagues in the BWH Department of Radiology to install a purpose-built MRI in BWH’s Newborn Intensive Care Unit. To be installed this summer, the scanner will facilitate Inder’s longitudinal study of premature babies born at BWH. She started similar studies earlier in her career, which involved scanning children’s brains at regular intervals, from birth into adulthood.
“Defining the injury can help inform prognosis and target treatments for babies. MRI does this far better than ultrasound,” says Inder. “We know the difference this kind of knowledge makes in helping adults recover from brain injuries. Imagine the effect it can have on a tiny baby at the beginning of their life. But to improve their future, we have to be willing to look.”

EXPANDING THE FRONTIER OF EPILEPSY CARE
Brain scans are an essential tool for determining the nature and treatment of many neurological conditions. For people with epilepsy, a neurologic disorder of recurrent seizures, an MRI of the brain can be the first step to finding relief, either through medication or surgery.
“Epilepsy is the fourth most common neurological problem, after migraine, stroke, and Alzheimer’s disease,” says Ellen J. Bubrick, MD, director of epilepsy surgery at BWH. “Unfortunately, one third of the 65 million people in the world with epilepsy don’t respond to any of the more than 20 medications now available.”
Uncontrolled, epileptic seizures can be debilitating and deadly. “More people die each year of seizure-related injuries than from breast cancer,” says Bubrick. “People with intractable epilepsy are also more vulnerable to depression, anxiety, and suicide. And we know that the earlier in the disease we can stop the seizures, the fewer cognitive and behavioral problems people will have. This is a patient population with a lot of suffering, sometimes over an entire lifetime.”
One third of the people whose epilepsy is resistant to medication can be significantly helped, or even cured, by surgery. But surgical success often requires seeing the epilepsy lesion on the brain, and MRI technology hasn’t always been up to the task.
The real voyage of discovery consists of not in seeking new landscapes but in having new eyes.
– Marcel Proust, French novelist, (1871-1922)
Bubrick is in the early phases of using a variety of imaging technologies to tackle the most intractable cases of epilepsy: inoperable and medication resistant. Magnet strength in MRI is measured in Teslas (or T), with lower numbers corresponding to lower resolution. With BWH’s new 7T MRI, one of the only 7T MRI machines in the nation installed in a clinical setting, Bubrick is locating previously undetected lesions in epilepsy patients, many of whom have experienced daily seizures for years with no relief.
“One patient came to me having endured daily seizures for most of his life,” Bubrick says. “His 3T scans looked normal, but when we put him through the 7T, everyone in the room could clearly see the lesion, how big it was, and exactly where it was. The 7T opened new doors, both in making him a surgical candidate and improving the surgery he got. He’s been seizure-free ever since his surgery. Being able to expand the frontier of treatment for people like him is deeply rewarding.”
Besides making epilepsy lesions more visible, the 7T is also improving the ability to read lower resolution scans.
“We are just at the beginning of learning what we can see with the 7T,” says Bubrick. “Beyond detecting new lesions, it’s helping us look at 3T and 1.5T scans in new ways, to see lesions we didn’t see before. This will help us teach people who don’t have access to a 7T how to better read lower resolution scans, to show them what to look for. Eventually, we hope to improve the reading of lower resolution scans, so you won’t have to have access to a 7T to see a lesion. That will be a huge step forward.”

VIRTUAL TOOLS IMPROVE PLANNING AND TREATMENT
Today’s state-of-the art digital scanning tools such as MRI and CT render sophisticated and detailed three-dimensional images built from layers of images called slices. However, most of these scans are viewed one slice at a time on computer monitors incapable of 3-D display. Radiation oncologist Konstantin Kovtun, MD, and medical physicist Christopher Williams, PhD, want to change that.
“The way clinicians and surgeons currently view 3-D imaging data diminishes its precision and context,” says Williams. “We want to optimize the way we look at and understand scanning data.”
Kovtun and Williams have adapted a commercially available HTC VIVE virtual reality (VR) headset to enable the viewing and manipulation of scans in their original 3-D format.
“When we started experimenting with the HTC VIVE, we saw that VR technology offers huge advantages for seeing and manipulating 3-D medical images,” says Williams.
In their roles in the Department of Radiation Oncology, Kovtun and Williams often collaborate to plan radiation delivery to cancer patients. By allowing them to see tumors in the context of surrounding tissue and bone, they believe VR technology could vastly improve radiation treatment safety and reduce the time it takes to plan radiation oncology sessions when compared to viewing scans one slice at a time.
One sees great things from the valley, only small things from the peak.
– G. K. Chesterton, British author (1874-1936)
“In radiation oncology, we deliver radiation from outside the body to target cancers inside the body,” says Kovtun. “We want to avoid hitting healthy tissue and important organs as much as possible. This VR system is a faster, and we think better, way to plan angles of delivery so it is the least deleterious to our patients.”
The duo’s conversations with neurosurgeons are widening the potential uses for their project. One possibility is to help plan for surgery for a brain aneurysm.
“With this system, a surgeon can look at the 3-D image of all the vessels in the area of an aneurysm, rotate it in six directions, zoom in and out,” says Williams. “You can use the controller to see how big a hole you’ll need to cut in the skull to get at the aneurysm. Being able to map your surgical approach more precisely, based on each patient’s anatomy before you open them up, we think could be really powerful.”
BUILDING THE TOOLBOX FOR PRECISION MEDICINE
Whether providing more precise diagnostics of injury and disease or offering improved guidance for treatments, imaging technologies give clinicians, surgeons, and scientists new ways of seeing and start them on the path of better understanding what they see.
“Technology is never our end goal in medicine,” says Di Carli. “It’s always about expanding our toolbox. The best tools are the ones that help us take care of our patients better. Today, imaging is a powerful tool for us. It gives us a window to peek inside without cutting people open.”